Abstract
Introduction: Acute Myeloid Leukemia (AML) is a heterogeneous disease affecting over 20,000 adults in the U.S. each year. People diagnosed with AML experience a period of shock compounded by the need to make quick treatment decisions. Coping not only with the direct symptoms of disease and treatment (e.g., fatigue, nausea, pain), but also lifestyle changes (e.g., inability to live independently, inability to conduct usual activities) is integral to the patient experience. Coping has also been shown to mediate the impact of integrated palliative care on improving outcomes. While several studies analyze coping mechanisms in AML using predetermined scales, less is known about how patients themselves describe their coping strategies when asked open-ended questions about their experience. We aimed to explore patients' coping methods, through their own words, using qualitative methods.
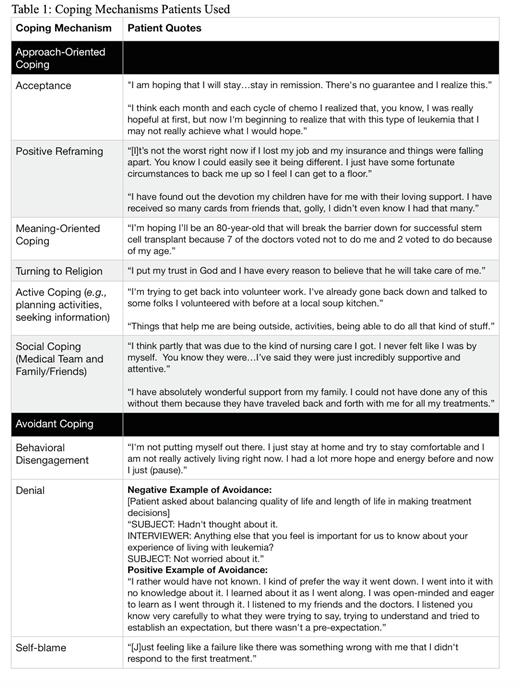
Methods: We enrolled patients with high-risk AML admitted to Duke Hospital's inpatient hematologic malignancy service for high dose chemotherapy treatment. This study is a secondary analysis of previously collected longitudinal qualitative data, with patient interviews conducted between February 2014 and March 2015 (up to three semi-structured interviews per patient). Interviews were coded in NVivo using open and axial coding to identify coping mechanisms. Coping mechanisms were divided into two broader categories: approach-oriented coping (acceptance, positive reframing, meaning-focused coping, relying on faith, active coping, and social coping) and avoidant coping (behavioral disengagement, self-blame, and denial).
Results: Of the 32 patients in the study, the mean age was 61.8 years. Similar proportions of patients in the study had normal karyotype (53.1%, n=17) and complex karyotype (46.9%, n=15) and most patients were newly diagnosed (68.8%, n=22). One approach-oriented coping strategy employed by patients was acceptance-accepting one's prognosis, consequent lifestyle changes, and new normal: "[I will] be monitored, y'know continuously for the rest of my life. I accept that." Others accepted the uncertainty of AML: "You don't know what to expect. You just go with the flow. There is no expectation with cancer." Many patients used positive reframing by keeping perspective, either by hypothesizing about how it could be worse or comparing their situation to others: "There are millions and millions of people who have so much less than I do, who are in such pain, who don't have roofs over their head." Other patients found greater admiration for activities previously taken for granted: "[AML] made me want to go back and appreciate some of the things that I didn't appreciate. Just a good long walk, working in the garden, being with my friends." Another coping strategy included deriving meaning from their own experience, either by focusing on lessons learned or feeling that they could help others. Finally, social coping fell into two categories: patients feeling support from their medical team and from their community. Notably, some also felt guilt for being a "burden" on family members who drive them to medical appointments and take care of them.
Avoidant coping mechanisms were present in the form of behavioral disengagement-pulling away from loved ones or feeling "numb," as well as self-blame when treatment did not work. However, the most common avoidant coping mechanism patients discussed was denial, either in the form of emotional suppression or manipulation of the truth, as is the case with a patient who stated, "I call it cured. Doctor said it's in remission, but I don't know. I call it cured." Yet, there were instances in which avoidance of full information appeared to be adaptive, for example if the patient decided to break their treatment into more manageable subsections: "If there's going to be several stages, let's focus on Stage 1 and get through it; there's a mile marker to get to where we are and then we will go on from there."
Conclusion: These results demonstrate the diverse applications of coping mechanisms in the wake of an AML diagnosis. Specifically, within broad categories of coping strategies (e.g., positive reframing), important subdivisions exist, and must be understood in order to best support patients. Future research should aim to further elucidate these nuances and how they affect the emotional wellbeing of patients.
Disclosures
Leblanc:GSK: Consultancy; Genentech: Consultancy; Pfizer: Consultancy; BeiGene: Honoraria; Flatiron: Consultancy; BMS/Celgene: Consultancy, Research Funding, Speakers Bureau; BlueNote: Consultancy; Astellas: Consultancy; Agios/Servier: Consultancy, Speakers Bureau; AstraZeneca: Consultancy, Research Funding; AbbVie: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal